
Sun safe: A brief primer on sunscreen for patients
By Dr. Esha Singh, ND
Features Photo: © M-Production / Adobe Stock
Photo: © M-Production / Adobe Stock When it comes to summer skin care and safety, sunscreen is one of the most important products that one can use. Not only does it decrease the risk of developing skin cancers and precancers, but it also protects against sunburns, signs of premature aging and hyperpigmentation. Despite it being such an accessible and fundamental tool, in my practice I have seen a great gap in knowledge on the proper application of sunscreen. In this article, I hope to highlight the role that Naturopathic and Chiropractic doctors can play in sunscreen education within their clinical practice, as well as the fundamental basics of sunscreen.
Role of Naturopathic and Chiropractic Doctors
Naturopathic and chiropractic doctors hold a unique position within the integrative healthcare model which allows for more time for health behaviour promotion. Given this opportunity, it is imperative to recognize the risk factors of developing skin cancer and understanding the protective benefits of sunscreen.
While a full skin examination is recommended as part of an annual health checkup, NDs and DCs should be regularly scanning the skin during general assessments and treatments.
When conducting a quick scan, check areas that are both exposed and not exposed to the sun. It is more common for skin cancer to develop on exposed areas, but 20% of melanoma can be found on non-exposed skin.
If a lesion is detected, going through the following 7-point checklist can help one assess whether a lesion is cancerous. (See figure 1, below.) Any mole/lesion that scores more than 3 points should be referred to a specialist. Furthermore, when educating patients on melanoma-detection, teaching the ABCDE’s of skin cancer is a useful tool.
Sunscreen and melanoma
Sunscreen’s main claim to fame is its ability to block ultraviolet light, and thus decreasing the risk of skin cancer. One of the most common types of skin cancer is melanoma. Melanoma is a group of four skin cancers that begin in the melanocytes. Melanocytes are the specific type of pigmented skin cell that give colour to the skin, eyes, and hair. A mole is a non-cancerous benign tumor formed by a group of melanocytes that coalesce together. Moles can be pink, tan or brown in colour, flat or elevated, and can appear throughout the body. While melanocytes are harmless, certain changes, such as excessive UV exposure, can cause the melanocytes to become cancerous. The four types of melanoma are superficial spreading melanoma (which is the most common), nodular melanoma, lentigo maligna melanoma, and acral lentiginous melanoma.
While the rates of many common cancers are decreasing, melanoma is among the few that are increasing. In 2021, it was estimated that 8700 Canadians would be diagnosed with melanoma and 1250 Canadians would die from it. When looking at the sex-distribution of melanoma, 4700 men would be diagnosed and 790 would die and 4000 women would be diagnosed and 450 would die. The lifetime risk of developing melanoma is 1 in 59 for men, and 1 in 73 for women.
Figure 1
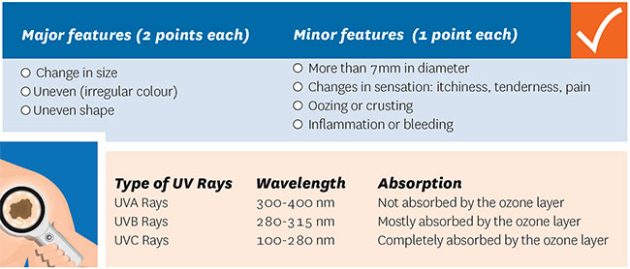
Photo: © rumruay / Adobe Stock
Risk factors for developing melanoma:
- Fair, sun sensitive skin that burns rather than tans; freckles; red or blonde hair
- More than 50 moles
- Moles that are large or unusual in colour or shape
- Family history of melanoma or a personal history of melanoma
- Excessive exposure to UV from sun or the tanning bed
- History of severe sun burns
Melanoma can develop in a matter of weeks and months, or can develop slowly over years. While tumours known to appear quite unusual in colour and shape, melanoma can also be unassuming and look like a normal mole or freckle. For men, the most common location of a melanoma is on the back, whereas women tend to develop it on their leg. Other common locations include the arms, scalp, and face. Individuals who have deeper skin tones may develop melanoma on the soles of their feet, toenails, or palms of their hands.
Ultraviolet radiation
One of the risks of developing melanoma is excessive ultraviolet radiation (UV) exposure. UV rays are non-ionizing radiation that are emitted from natural (i.e. the sun) and artificial light sources. Artificial sources of UV rays include tanning beds; mercury vapor lighting found in school gyms and stadiums; halogen, fluorescent, and incandescent lights; and certain types of layers. There are three types of UV rays that are emitted from these sources: UVA, UVB, and UVC. Of these types, we are most concerned about UVA and UVB rays.
Figure 2.

Photo: © rumruay / Adobe Stock
In general, the harm caused by UV rays is greater than the benefit, so efforts must be made to avoid excessive exposure. The main benefits of UV rays are 1) the mediation of Vitamin D production and 2) endorphin production in the skin. For these reasons, the World Health Organization recommends 4-15 minutes of sun exposure 2-3 times per week. The risks associated with excessive UV exposure include: sunburns; premature aging; increased sensitivity to UV rays when on certain medications or topical products; and increased reishi of potentially blinding eye diseases.
UVA rays have a longer wavelength compared to UVB rays and thus, are able to penetrate deeper into the skin. This penetration increases the risk of genetic damage in cells in the depression layers of the epidermis. When there has been excessive exposure to UVA rays, the skin starts to tan. Tanning is a protective mechanism that occurs in response to sun damage. The skin darkens itself to prevent further damage. UVA rays are associated with premature aging (think UV Aging) and has been linked to the development of skin cancer. UVA rays are not seasonal and are present during the cloudiest days in the winter. UVA rays are also able to penetrate windows.
UVB rays have a shorter wavelength than UVB and affect the outermost layers of the skin. UVB rays are associated with suntans, sunburns, and skin blistering (think UV Burning). UVB rays are associated with SPF (sun protection factor): a rating that tells us how effective particular sunscreen is against UVB rays. The strength of UVB rays fluctuates with the time of day with the highest risk of damage between mid-morning to mid-afternoon from Spring-Fall.
Sunscreen, sunblock or suntan lotion, is a photoprotective product that has the ability to absorb or reflect a portion of the sun’s UV rays. It can come in many different formulations including lotions, sprays, tells, foams, sticks, and powder. Sunscreen can also be added to clothing such as sunglasses, sunhats, and other sun protective clothing.
The use of photoprotective products dates back to at least the ancient Egyptian civilizations. There is evidence that they used ingredients such as rice bran, jasmine, and lupine to protect themselves from the rays of the sun. The first sunscreen was invented in Australia in 1932 by the chemist, H.A. Milton Blake. He created a UV filter called ‘salol, or phenyl salicylate, at a 10% concentration.
 There are two main types of sunscreens available on the market today: inorganic and organic sunscreen. Both forms work by absorbing UV light and converting it to heat.
There are two main types of sunscreens available on the market today: inorganic and organic sunscreen. Both forms work by absorbing UV light and converting it to heat.
Inorganic sunscreen, which is often mistakenly referred to as ‘physical sunscreen’, is made up of minerals/ionic compounds such as zinc oxide or titanium dioxide. Inorganic sunscreen was originally thought to work by scattering and reflecting UV rays. Newer studies found that inorganic sunscreens may absorb up to 95% of UV light, deflecting only about 5%
Organic (chemical) sunscreens consist of molecules with a carbon-chain structure. They work by absorbing UV light, converting them to heat, and then releasing them from the body. While there are many chemical sunscreen filters in the European/Asian market, only 17 are approved in Canada. These include homosalate, Mexoryl SX, Mexoryl XL, and avobenzone.
Resources:
- American Academy of Dermatology Association. Skin Cancer Types: Melanoma Signs and Symptoms. www.aad.org Accessed March 20, 2022.
- Azoury SC, Lange JR (October 2014). “Epidemiology, risk factors, prevention, and early detection of melanoma”. The Surgical Clinics of North America. 94 (5): 945–62, vii.
- Canadian Cancer Society. Melanoma skin cancer statistics. www.cancer.ca. Accessed March 20, 2022
- Cole, Curtis et al. “Metal oxide sunscreens protect skin by absorption, not by reflection or scattering.” Photodermatology, photoimmunology & photomedicine vol. 32,1 (2016): 5-10. doi:10.1111/phpp.12214
- Edlich, Richard F et al. “Photoprotection by sunscreens with topical antioxidants and systemic antioxidants to reduce sun exposure.” Journal of long-term effects of medical implants vol. 14,4 (2004): 317-40.
- Kanavy HE, Gerstenblith MR (December 2011). “Ultraviolet radiation and melanoma”. Seminars in Cutaneous Medicine and Surgery. 30 (4): 222–8.
- Matta, Murali K et al. “Effect of Sunscreen Application on Plasma Concentration of Sunscreen Active Ingredients: A Randomized Clinical Trial.” JAMA vol. 323,3 (2020): 256-267. doi:10.1001/jama.2019.20747
- Nadim S (2005). “Sunscreen Evolution”. In Shaath N (ed.). Sunscreens : regulations and commercial development (3 ed.). Boca Raton, Fl.: Taylor & Francis.
- Norval M, Wulf HC (October 2009). “Does chronic sunscreen use reduce vitamin D production to insufficient levels?”. The British Journal of Dermatology. 161 (4): 732–6.
- Rigel, Darrell S.; Weiss, Robert A.; Lim, Henry W.; Dover, Jeffrey S. (January 30, 2004). Photoaging. CRC Press.
- Sander, et al. The efficacy and safety of sunscreen use for the prevention of skin cancer. CMJA 2020; 1802-1808.
- Skin Cancer Foundation. www.skincancer.org Accessed March 20, 2022.
- World Cancer Report 2014. World Health Organization. 2014. pp. Chapter 5.14.
DR. Esha singh is is a naturopathic doctor practicing in Vancouver, BC. She has a clinical focus in skin health and uses an integrative approach to clinical dermatology. Dr. Esha strives to make information on skin health simple and accessible.
Print this page